Comfort posthectomy
Professor Hersant - Human Surgery at Paris Est Créteil
Introduction
Posthectomy or circumcision is an operation involving partial or total removal of the foreskin, a tissue composed of skin (outer layer), mucous membrane (inner layer), nerves, blood vessels and muscle fibres. The foreskin is connected to the glans by the frenulum, a thin strip of tissue that limits its movements and allows it to be returned to its basic position above the glans.
Circumcision is a surgical procedure that is frequently performed for religious, medical or aesthetic reasons. According to the World Health Organisation (WHO), in 2009, 661 million men over the age of 15 were circumcised, representing around 30% of the world’s male population(1).
Anatomy
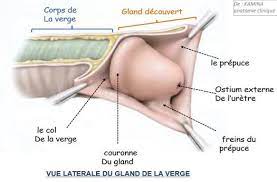
Figure 1: Side view of the glans penis and foreskin.
The foreskin is formed by the various envelopes of the penis, which form a cylindrical fold around the glans. The foreskin forms a sleeve around the glans. On the underside of the glans is a fold of skin that connects the foreskin to the base of the glans: this is the foreskin frenulum. At the base of the glans, there is a circular relief, the crown of the glans, which defines the balanopreputial fold underneath.
Indications
There are a number of indications for this operation: treatment of phimosis (glans completely covered when erect), or a foreskin that is too tight, making unhooding difficult or impossible. This causes hygiene problems that can be complicated by local superinfections (balanitis, balanoposthitis) or even chronic inflammation, as well as urinary tract infections. The condition is virtually constant in infants, and should only be operated on if it persists beyond the age of 4 or 5, following medical treatment with local corticosteroids.
Other indications include conservative surgery for localised, early-stage preputial tumours. For religious reasons in young children or in adults in the event of conversion. Or for aesthetic reasons.
It is most often performed during childhood for religious reasons or to reduce the frequency of recurrent local or urinary tract infections, but also in young adults and the elderly. Aesthetic circumcision is intended solely to correct the appearance of the penis, with the glans partially or totally uncovered at all times, even when at rest. In addition to the cosmetic changes, circumcision is said to reduce the risk of sexually transmitted infections, in particular the human immunodeficiency virus (HIV)(2).
The WHO currently recommends posthectomy to reduce the risk of transmission of infectious diseases. Post-hectomy is widely performed in the USA and Africa. However, the European Society of Sexual Medicine does not recommend this practice, which in the absence of medical indication is considered genital mutilation(3).
Contraindications
The contraindications are patients who, when erect, have a totally uncovered glans and a completely lifted sheath. This means that the preputial skin reserve is necessary to support the erection. A posthectomy in this context may result in a shortening of the erect penis. Total posthectomy is therefore contraindicated for aesthetic purposes. We can only suggest a partial posthectomy to avoid any consequences on the erection: shortening, pain during intercourse, scarring.
Surgical technique
This diagram corresponds to the total posthectomy indicated in pathology. This procedure is contraindicated in aesthetic surgery.
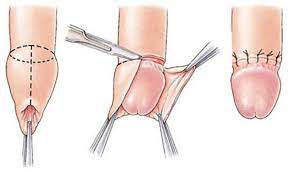
Figure 1: total posthectomy
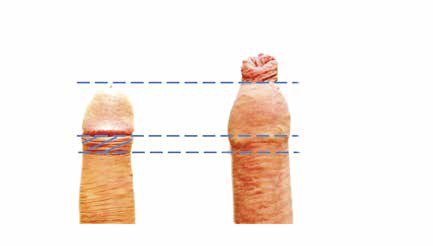
Figure 2: partial posthectomy: this procedure is preferred: in 1, with the penis unwrapped, the prepuce can be seen wrinkled at the balanoprepucial fold. In 2, in the recall position, only the part of the prepuce extending beyond the glans needs to be respected.
This short procedure, lasting around 30 minutes, can be performed under general anaesthetic, local anaesthetic or penile block. The patient lies on his back with his arms at his side.
The operation consists of a mucocutaneous resection of the distal part of the penis. Several techniques are possible(4), one of which begins with a line drawn on a cushioned penis opposite the balanopreputial fold (5mm below the crown), followed by a pinch-test to determine the limits of the resection, this time on a cushioned penis in order to adapt the amount of tissue excised to the desired result (Figure 2).
Finally, the suture between the sub-balanic mucosa (Figure 1) and the skin of the penis is made using separate stitches of rapidly absorbable thread. There are different types of circumcision, depending on the proportion of foreskin skin and mucosa removed and the location of the scar. For aesthetic reasons, the stitches should be carefully separated without overlapping the edges to avoid cysts, skin bridges and unsightly scars.
The suture must be made between the mucous junction of the balanopreputial fold and the skin of the sheath. In all cases, the glans penis can be retained or removed. In this case, the scar is barely visible as the skin falls back over the glans at rest and there is usually enough skin left to allow the penis to slide.
Post-operative care
A dressing with a greasy interface is made up at the end of the operation and removed the day after by the patient or a nurse. After the operation, care is limited to daily hygiene of the surgical wound with soap and water. A period of sexual abstinence of at least 3 weeks is required to allow the wound to heal properly.
Complications
Although circumcision is a common practice, it carries a number of risks 5, as does any surgical procedure, and requires a certain amount of experience in order to optimise aesthetic results and limit post-operative complications. The overall rate of early complications is low. The main complications are post-operative haematoma, surgical site infection, delayed healing and aesthetic dissatisfaction. The main risks in the case of radical or total posthectomy are shortening during erection, pain during intercourse and scarring.
Bibliography
1. Male circumcision: global trends and determinants of prevalence, safety, and acceptability. Geneva: World Health Organization: UNAIDS, 2008.
2. Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2(11):e298. doi:10.1371/journal.pmed.0020298
3. Communiqué de presse : l’OMS et l’ONUSIDA annoncent des recommandations émanant d’une réunion d’experts sur la circoncision masculine et la prévention du VIH. data.unaids. org/pub/pressrelease/2007/070328_pr_ mcrecommendations_fr.pdf.
4. Holman JR, Stuessi KA. Adult circumcision. Am Fam Physician. 1999;59(6):1514-1518.
5. Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction?–a systematic review. J Sex Med. 2013;10(11):2644-2657. doi:10.1111/jsm.12293
