Hymenoplasty
Professor Hersant - Intimate Surgery Paris Est Créteil
Hymenoplasty
This chapter is devoted to hymenal reconstruction by hymenoplasty. This procedure is particularly controversial because of its ethical implications(1). We have chosen to treat this subject in the same way as any other genital plastic surgery procedure, because it is important for all plastic surgeons to be familiar with the anatomical and surgical basis of this region, as it is frequently requested in certain ethnic communities.
We would remind you that it is forbidden to issue a medical certificate of virginity in France. Hymenoplasty or surgical restoration of the hymen is one of the least described surgical procedures in plastic surgery(2). There is no reference technique. In view of the small number of publications, this chapter describes the different hymen restoration techniques.
Anatomy
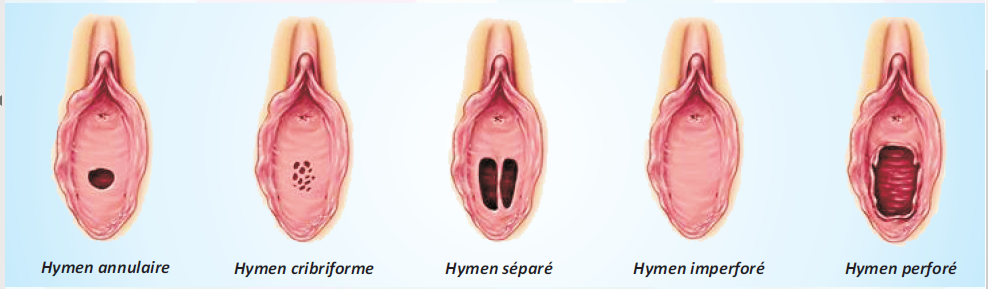
Figure 1: The different types of hymen
The hymen is a thin membrane made up of mucous folds that partially close the vaginal orifice. This membrane is actually an embryonic remnant from the urogenital sinus. It is perforated to allow the evacuation of blood at the time of menstruation. The hymen is mainly composed of elastic connective tissue and collagen. It is covered on both sides by stratified squamous epithelium. Its shape varies greatly from one woman to another(3).
There are different types of hymen (Figure 1):
- Imperforate hymen: membrane that covers the entire entrance to the vagina.
- Micro Perforated hymen: the membrane almost entirely covers the entrance to the vagina; the perforation of the hymen is very small.
- Bifenetrate hymen: the membrane has two small openings in the vagina instead of one.
- Cribriform hymen: membrane with multiple small holes.
- Sclerotic hymen: thick, resistant membrane which hinders sexual relations.
- Complacent hymen: elastic membrane that dilates without bleeding or tearing.
- Absent hymen
During adolescence, its elasticity increases considerably.
There is no recognised specific function for the hymen. It may, however, protect the vagina from faecal matter and other contamination at the start of life. When it ruptures, the hymen appears in the form of mucosal folds located circumferentially at the level of the introitus. Over time, the angular margins are smoothed. Bleeding from the hymen when it ruptures is not systematic.
Ethical approach
Although the definition of virginity can be contested, many people wrongly consider an intact hymen to be the sine qua non of sexual chastity.
For many cultures, the presence of an unbroken hymen is synonymous with morality, honour and integrity. These beliefs can cause anguish and suffering for young women from certain communities. The fear of being rejected by the community and family is such that some women resort to this type of procedure even in this day and age(4).
Hymenoplasty can sometimes be covered by social security in special paediatric plastic surgery situations, particularly after physical trauma (accident, sexual abuse, etc.).
Indications
Most requests for hymen reconstruction are made in the context of a forthcoming wedding, in order to prove virginity on the wedding night. There may be other reasons for the request, such as a relationship breakdown, a history of rape or fear of family reprisals.
Leaving aside the ethical context, anyone who presents with realistic expectations and who has sufficient hymenal tissue is a candidate for hymenoplasty. Variations in technique can be performed for patients with insufficient hymen fragments.
Contraindications
Contraindications to hymenoplasty are rarely absolute and often transient. The main contraindications are active vulvovaginal infections, active vulvovaginal inflammatory conditions, unlabelled metrorrhagia, pregnancy, coagulopathy and active smoking.
Today we are faced with new and ‘exotic’ requests: couples wishing to relive ‘a first time’, physical restoration after adultery, women symbolically wishing to make a fresh start after divorce. These are clearly symbolic requests. In these cases, surgery is contraindicated, but the patient should be referred for psychological and sexological treatment, as the psychological suffering is real.
Preoperative preparation
There is no pre-established tool for assessing candidates for hymenoplasty. The hymen has no standard appearance and a wide variety of anatomical variations have been described. Furthermore, the optimal diameter or size of the hymen has not been determined by studies. There is no standard hymen that can be reproduced or reconstructed.
Two main types of technique may be proposed, depending on the time available. A hymenorrhaphy will be performed if the delay is less than 15 days, whereas a hymenoplasty may be performed if the delay is more than 15 days.
It is also necessary to explain the principles of the surgical procedure to the patient, if necessary with the help of a mirror, in order to show her what is possible and what is impossible, so that her expectations are not unrealistic.
It is also crucial to take into account the degree of insecurity of the environment in which the patient is living, in order to protect her as best as possible.
Surgical techniques
In the absence of a standard hymenal aspect, several surgical techniques have been described with the main objective of restoring a narrow membranous introitus.
In most reviews, the surgical technique is vaguely described and success rates are rarely quoted. However, the approaches to this surgery can be classified as follows(5) :
- Simple hymenal suture (hymenorrhaphy)
- Hymenal repair using a flap (Placik technique)
- Simple approximation of hymenal vestiges by suture after de-epithelialisation: hymenoplasty
- Hymenoplasty and perineoplasty are performed most frequently in the Maghreb and the Middle East to guarantee bleeding on the day of intercourse. We do not recommend this procedure, which carries a risk of subsequent obstetric trauma.
Whatever the technique used, it is important to systematically preserve an outlet for vaginal discharge and not to perform a plasty on the urinary meatus in order to protect it from any damage.
Anaesthesia
A number of anaesthetic techniques can be used. The patient may be offered the following techniques: general anaesthesia, local anaesthesia combined with sedation, spinal anaesthesia, pure local anaesthesia.
Simple hymenoplasty :
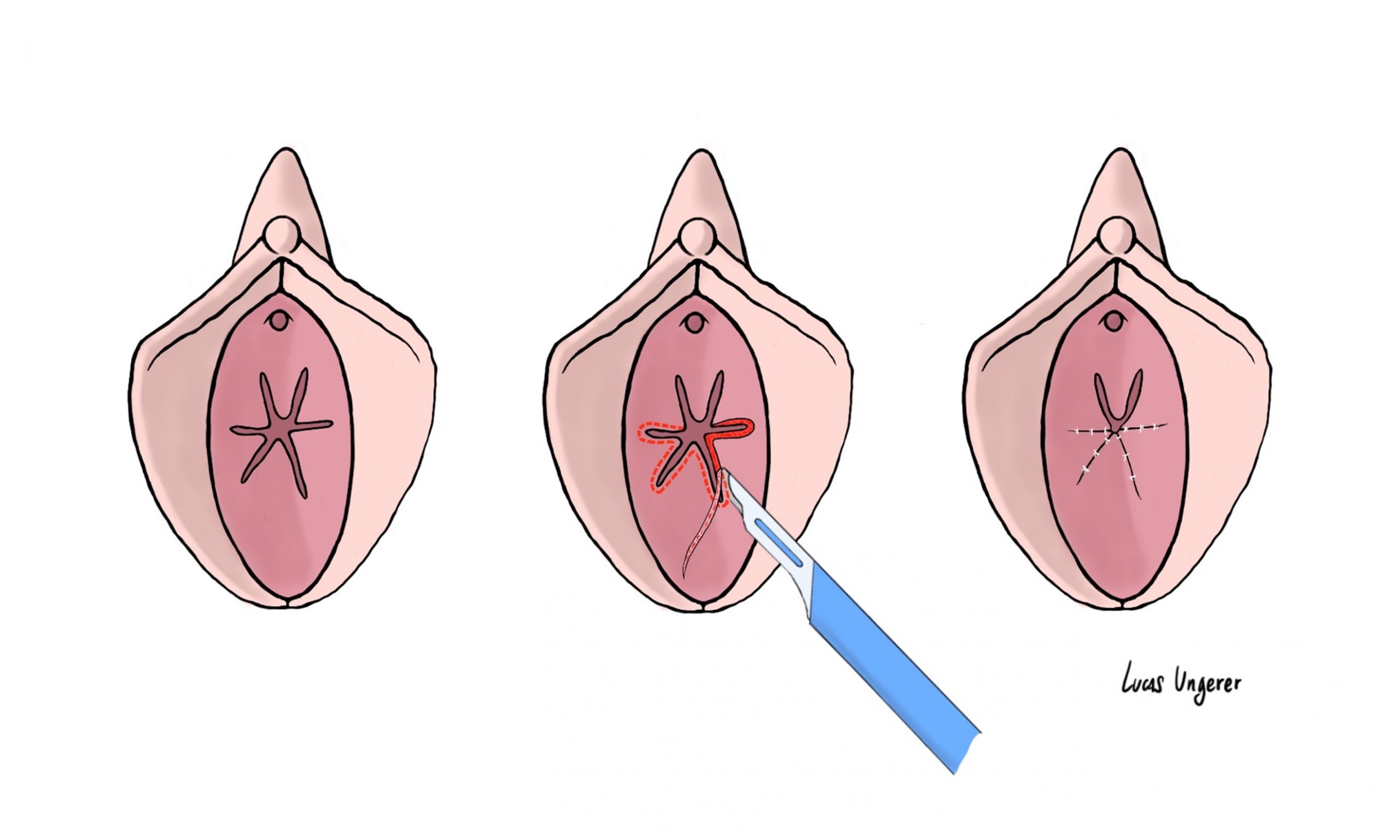
Figure 2: Simple hymenoplasty technique
The patient is systematically positioned in the gynaecological position.
This technique involves firstly incising all the free edges of the various hymenal remnants, removing the superficial mucous area in order to brighten up the free edge. The free edges are then sutured together using a double hemi-suture of Vicryl or colourless monocryl 5/0, leaving a small hole in the neo-hymen in the upper third to avoid any risk of urinary complications.
Hymenoplasty using hymenal flaps
Use of this technique requires the presence of sufficient hymenal caruncles. The technique begins by incising the free edge of the hymenal remnants in order to separate the external mucosa from the internal mucosa of the hymen. The inner hymenal mucosa is then peeled away with Metzenbaum scissors down to the vaginal mucosa. Dissection continues under the posterior vaginal mucosa, which is peeled back about 2 cm.
This dissection allows us to reach the pararectal fossae, which are also dissected to reveal the levator muscles. These two muscles are then brought together to narrow the introitus using two stitches of Vicryl 1 on the midline. Next, the two hymenal flaps are sutured edge to edge with an overjet of colourless Vicryl 4/0, while the needle is passed deeply to attach the neo-hymen to the newly brought-together muscles.
Hymenoplasty using vaginal flaps

Figure 3: Hymenoplasty using vaginal flaps
This technique does not require the presence of hymenal remnants (Figure 3). It is therefore preferred when hymenoplasty using hymenal flaps is not feasible.
The procedure begins with a vertical incision of the posterior vaginal mucosa from the hymen to a depth of approximately 2 to 3 cm. The vaginal wall is then dissected into two flaps ranging from 6 to 10 hours on the right and from 6 to 2 hours on the left. The pararectal chambers are then dissected in order to perform perineorrhaphy by suturing the 2 levator muscles with two stitches of Vicryl 1. The outer surface of one of the two flaps is de-epithelialised using fine scissors. This is then folded over the fixed base of the other flap and sutured with colourless Vicryl 4/0. The second flap is then folded over the previous one and sutured to it with colourless Vicryl 4/0.
We do not recommend this technique, which may cause obstetric problems.
Post-operative follow-up
The post-operative recommendations are to avoid any position in which the thighs overlap or are as far apart as possible. Avoid any abdominal hyperpressure (light laxatives may be prescribed for 15 days). The use of a tampon should be avoided, as should self-examination to check healing. Wound care consists of spraying with saline or water as required.
Patients are encouraged to take showers and let soap and water run over the wound. However, bathing is totally contraindicated. Patients should not use public swimming pools, spas or saunas for 4 weeks. Physical activity should be limited for 4 weeks.
Results
The results of these repairs are extremely difficult to assess due to the lack of follow-up. As a result, ‘success’ rates vary and are very difficult to assess depending on the technique.
Bleeding at first intercourse is not systematic with the above techniques.
Complications
Few complications have been described concerning hymenoplasty. Most authors report that complications are minor. However, some mention the risk of secondary dyspareunia or difficulties with penetration. The most frequently reported complication is scar dehiscence. Studies report bleeding in only 50 to 67% of cases after hymenal restoration.
Finally, more serious complications such as post-operative haemorrhage and infection can sometimes occur, but their incidence remains to be assessed. Techniques combining vaginal flaps or perineoplasty may cause obstetric complications.
Bibliography
- O’Connor M. Reconstructing the hymen: mutilation or restoration? J Law Med. 2008;16(1):161-175.
- Goodman MP. Female genital cosmetic and plastic surgery: a review. J Sex Med. 2011;8(6):1813-1825. doi:10.1111/j.1743-6109.2011.02254.x
- Stewart ST. Hymenal characteristics in girls with and without a history of sexual abuse. J Child Sex Abuse. 2011;20(5):521-536. doi:10.1080/10538712.2011.606106
- Cook RJ, Dickens BM. Hymen reconstruction: ethical and legal issues. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2009;107(3):266-269. doi:10.1016/j.ijgo.2009.07.032
- Lahlali A, Sawan D, SidAhmed-Mezi M, Meningaud JP, Hersant B. Hymen Restoration: An Experience From a Moroccan Center. Aesthet Surg J. 2021;41(12):NP2053-NP2059. doi:10.1093/asj/sjab276
