Reduction Nymphoplasty
Professor Hersant - Women's surgery at Paris Est Créteil
Introduction
Reduction nymphoplasty is the most widely performed genital plastic surgery procedure in the world today. It consists in reducing the size of the labia minora by removing the excess mucosa. Labia minora hypertrophy is defined as the excessive size of the labia minora in relation to the labia majora. Demand for this type of surgery is growing year on year, and it is important for every surgeon performing this type of procedure to have a thorough knowledge of the anatomical area and the surgical implications.
There are a large number of techniques described for reduction nymphoplasty. However, two main techniques are currently used: wedge reduction and longitudinal resection(1). The advantages and disadvantages of each technique should be taken into account before proposing them to patients.
Labia minora hypertrophy is defined as an increase in the size of the labia minora. However, there is considerable inter-individual variation, and it is difficult to propose a standard in this area. The perception of the “normal” appearance of the labia minora is particularly influenced by cultural considerations, including exposure to pornography(2), although this theory has recently been debated(3).
Anatomy and physiology
Embryologically, the labia majora in women are derived from the genital folds that give rise to the scrotum in the male foetus. In contrast, the labia minora develop from the genital folds, which in the male foetus fuse to form the median raphe.
The labia minora are hairless mucocutaneous folds containing sebaceous glands. They continue with two extensions at the top to form the frenulum beneath the clitoris, and the clitoral hood which covers the clitoris(4).
The average size of the labia minora is 2 cm, but this figure can vary from 7 mm to 5 cm.
The labia minora play two key roles in women’s lives, and should be preserved during surgery. They prevent vaginal dryness and help to guide the flow of urine once it has left the urethra. During nymphoplasty surgery, it is important to leave a labia minora of more than 1 cm in place, and not to exceed Hart’s line (the dividing line between the labia minora and the vestibule) during mucocutaneous resection.
In fact, the vulvar vestibule extends laterally from the hymenal ring to a line of more keratinized mucosa at the level of the labia minora: this is Hart’s line(5). The sebaceous glands generally stop midway along the surface of the labia minora, this line corresponding to the boundary between the mucosa and the squamous epithelium.
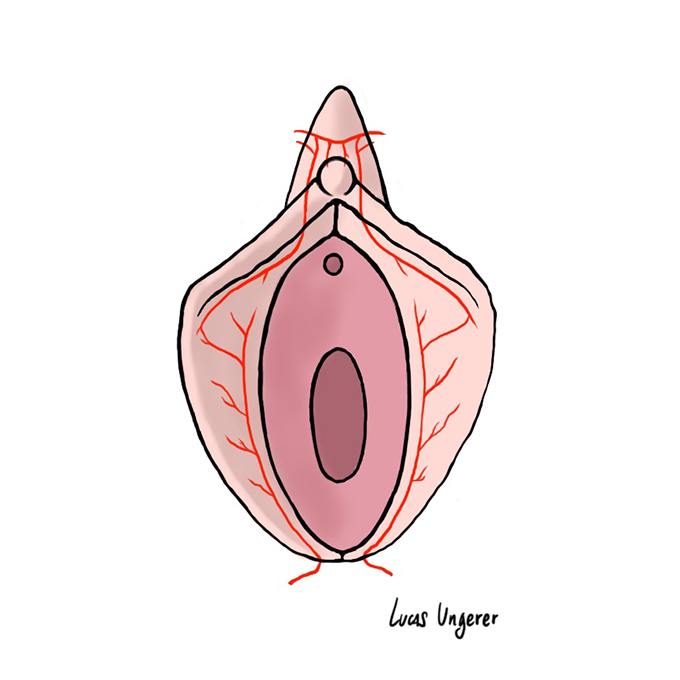
Figure 1: Anatomy of the arterial vascularization of the labia minora, with predominance of the superior vascularization.
Vascularization of the labia minora is achieved by a vascular network between the internal pudendal artery and the external pudendal artery. The anterior surface of the labia minora is supplied by branches of the external pudendal artery, while the posterior surface is vascularized by branches of the internal pudendal artery. Vascularization of the labia minor is distributed over its surface via three transverse arterial branches. The internal pudendal artery also supplies branches to the clitoral hood.
Venous return is via the internal pudendal vein and the vaginal venous plexus.
In terms of innervation, the anterior surface of the labia minora is innervated by branches of the ilioinguinal nerve (T12-L1) and the genitofemoral nerve (L1-L2). The posterior surface is innervated by branches of the internal pudendal nerve (S2-S4).
Finally, it’s important to know that the clitoris lies just below the clitoral hood. This is innervated by the dorsal clitoral nerve, which has two branches running at 11 and 1 o’clock to the body of the clitoris(6). It is crucial not to damage these two nerve branches, as this can lead to complications which can be dramatic for women (loss of sensitivity, neuroma).
Classifications
There are two main classifications that can be used to classify the degree of labia minora hypertrophy, as well as the location of the hypertrophy: Motakef’s classification (Figure 2) and Banwell’s classification(7). These two criteria may have an impact on the choice of resection technique.
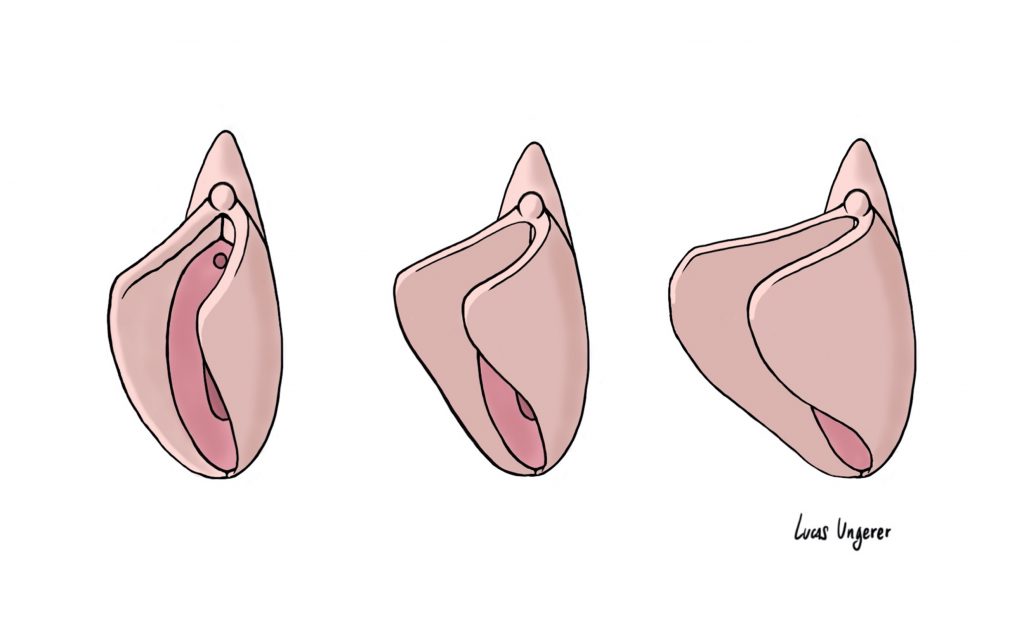
Figure 2: Motakef classification. It classifies labia minora into 3 categories according to length. Class I: 0 to 2 cm, Class II: 2.to 4 cm, Class III: over 4cm.
Indications
The main indications for labia minora reduction are as follows:
- Aesthetic discomfort: folded, asymmetrical or oversized labia minora
- Physical discomfort: when walking, playing sports, wearing tight clothing
- Sexual discomfort: pain during intercourse (superficial dyspareunia) due to penetration of the labia minora into the vulvar vestibule.
These indications are subjective, and it’s important to remember that there is no such thing as an “abnormal” labia minora, but rather variations around what might be called the “norm”. It is therefore important to rely on the patient’s own experience, and to take into account her history and feelings. It is also important not to over-indicate by proposing nymphoplasty in a patient who has no real request in this respect. These discomforts can lead to psychological problems and a reduced quality of sexual life(8).
Contraindications
The main contraindications to reduction nymphoplasty are insufficient length of the labia minora. Indeed, there is a risk of leaving an undersized labia minora, particularly by resecting the latter beyond Hart’s line, and thus impairing its function.
Smoking is also a contraindication to nymphoplasty, especially when the wedge technique is used, as resection takes place in an area of poor vascularization.
As with any plastic surgery operation, the patient’s overall assessment must be carried out, and any dysmorphophobia eliminated.
The Royal Society of Gynaecology and Obstetrics of Great Britain has expressed reservations about the practice of nymphoplasty in minors, due to the explosion in the number of procedures in the under-15 age group. As with any operation on the primary or secondary sexual organs, it’s best to wait until puberty and growth are over.
Pre-operative preparation
When assessing patients for labial surgery, it is essential to understand their goals and expectations. Questioning should focus in particular on the patient’s sexual and gynaecological history. It is important to describe the anatomical basis to the patient.
Examination of the genitalia is crucial, with assessment of labia minora size, asymmetry and pigmentation. It can be particularly useful to provide the patient with a mirror so that she can participate in the surgical planning. Gynaecological and standing photographs are mandatory (with the patient’s consent).
Smoking must be stopped at least 1 month before the operation to limit any vascular risk. No medication containing aspirin should be taken in the 10 days prior to the operation. Remember that the labia minora are hairless, so depilation is not necessary in this area.
Anaesthesia
The procedure is generally performed on an outpatient basis. Anesthesia can be chosen at the convenience of the patient and surgeon. The procedure can be performed under pure local anesthesia, local anesthesia combined with sedation, spinal anesthesia, or even general anesthesia for greater comfort.
Surgical technique: the wedge technique
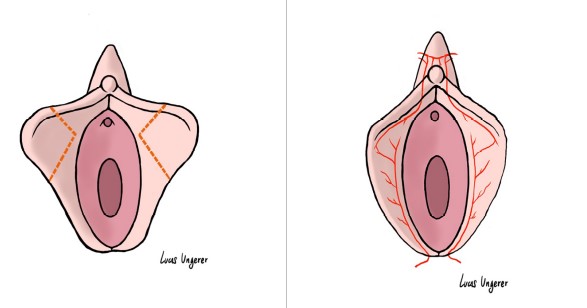
Figure 3: Wedge resection technique
La technique wedge (Figure 3) convient davantage aux patientes présentant un allongement radial des petites lèvres et qui présentent une pigmentation continue des bords. En effet, le tissu réséqué correspond à la partie la plus protubérante des petites lèvres. La partie supérieure et inférieure de la petite lèvre étant remises en continuité, il est important que la coloration soit identique afin de ne pas créer de discontinuité chromique(9).
Les marquages sont réalisés avant l’infiltration. La branche supérieure de V doit être placée au niveau supérieur de l’excès cutanéo-muqueux et la branche inférieure au niveau du pôle inférieur de l’excès. La branche antérieure ne doit pas être placée trop proche du méat urétral (plus de 0,5 cm) afin de ne pas entrainer de rétractions à ce niveau. Les deux bords du V doivent pouvoir se rapprocher l’un de l’autre avec une tension minimale. Il est important de reporter le dessin sur chaque face des petites lèvres de manière symétrique.
L’incision initiale est cunéiforme au niveau du versant cutané en externe et muqueux en interne au centre de la petite lèvre. Il est ensuite réalisé une exérèse de l’excédent cutanéo-muqueux. On peut s’aider de deux pinces de Kocher placées en dessous de chaque branche du V afin de réaliser la résection à la lame froide le long de chaque mords de la pince. Par la suite, il est important de réaliser une bonne hémostase à la pince bipolaire afin d’éviter toute formation d’hématome post-opératoire. Certains préconisent une désepithélialisation de V pour laisser en continuité le plan profond de tissu conjonctif.
La fermeture est le point le clé de l’intervention car le risque de désunion est important.
Si on pratique une désépthélialisation du V, alors 2 surjets seront à réaliser ; si on pratique on résection cutanéo-muqueuse, on doit réaliser 3 surjets : un interne sur le plan conjonctif de monocryl ou vicryl 4/0 incolore ; un plan superficiel externe par du moncryl ou vicryl rapide 4/0 et un plan superficiel interne par du vicryl rapide 4/0.
Surgical technique: the longitudinal resection technique
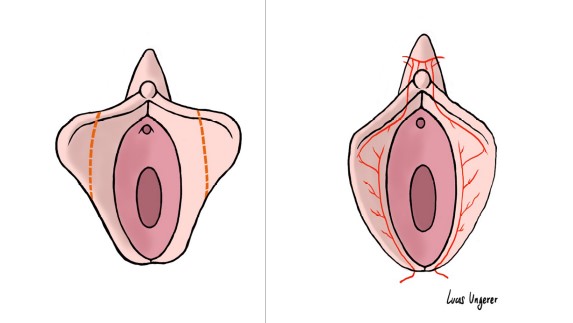
Figure 4: Linear resection technique
The linear resection technique of the free border of the labia minora may be suitable for a wide variety of labia minora, particularly those with discontinuous border pigmentation, unlike the wedge technique (Figure 4). It is also more suitable for women with a higher local vascular risk.
Markings are made with a surgical marker. Resection begins laterally and below the frenulum, extending to the vaginal orifice inferiorly. It is important to mark both sides of the labia minora, so as not to deviate in the subsequent resection. Conservative placement of the markings is recommended, as it is preferable to leave more labia than to remove excess. In order to obtain the most natural final shape possible, marking should be curvi-linear, with the external convexity placed at the level of the upper 1/3 of the labia minora. Resection can be more extensive on the medial side, while leaving a slightly wider lateral side to position the scar internally, so that it is not directly on the free edge (less visible internally). It is extremely important to leave at least 1 cm of labia minora and not to exceed Hart’s line during resection.
A Gillis hook is placed at each end of the free edge of the labia minora. The incision is made with a cold blade on each side of the labia minor according to the pre-operative drawings. Resection is then performed with a colorado tip or radiofrequency. Careful hemostasis with bipolar forceps is required. Closure is achieved with a submucosal overjet of Monocryl 4/0, followed by a cutaneous-mucosal overjet of colorless Vicryl 4/0.
Post-operative care
Post-operative care consists of daily saline cleansing after each toilet visit. Wearing loose-fitting cotton panties is recommended for 1 month. Sexual relations should also be suspended for 1 month.
Results
Results can be assessed 3 to 6 months after the procedure. Some patients experience significant oedema for several months, particularly those with vulvar varicose veins and those who have had significant oedema after childbirth. Scars fade within 3 months, and the vulva regains a harmonious shape in line with the patient’s wishes. Residual asymmetries are frequently present, but do not compromise the aesthetic result. Occasionally, resection may be insufficient, and secondary surgical correction may be required after 6 months to 1 year. In cases of associated hypotrophy, we recommend lipofilling of the labia majora(10) to improve the cosmetic result.
Some authors have demonstrated that lipofilling of the labia majora reduces the need for resection of the labia minora(1).
Analysis of the clitoral hood is important; it is often hypertrophic, and duplication may be observed. In this case, the excess can be corrected by a chevron plasty of the clitoral hood, while maintaining 5 mm from the free edge of the clitoral prepuce. Bipolar haemostasis is mandatory to avoid any diffusion towards the clitoris, so as not to damage the two branches of the dorsal nerve of the clitoris, which run at 11 and 1 o’clock on the body of the clitoris. Closure with separate stitches of colorless 4/0 rapid vicryl.
Herringbone plasty of the clitoral hood
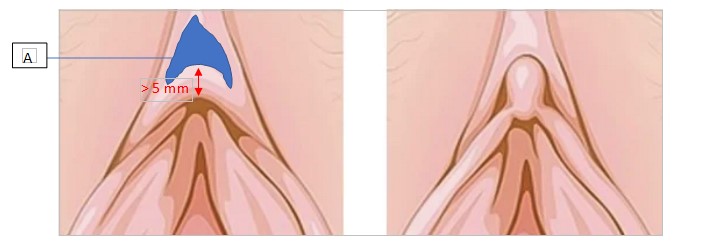
Figure 4: Linear resection technique
The clitoral hood varies anatomically from woman to woman. It can sometimes have a very large cutaneous portion, completely covering the clitoris. Some women complain of difficulties in clitoral stimulation at this level. In such cases, a herringbone plasty of the clitoral hood may be suggested. This is a simple technique, but not trivial, as the two branches of the dorsal clitoral nerve run along the upper part of the clitoral body (branching off and burying themselves in the clitoral glans). A distance of 5 mm from the free edge of the clitoral prepuce must be maintained.
The pattern of the plasty takes on a “chevron” or “gendarme hat” shape (Figure 5). The area is then de-epidermized. Suturing is performed using simple 4/0 Vicryl rapid stitches. Resection will enable the cap to be re-tensioned and the glans penis to be uncovered.
Complications
The main complication of nymphoplasty is dehiscence of the post-operative scar, particularly in patients who smoke. This is a much more frequent complication when the wedge technique is used, due to the presence of the scar in the area of poor vascularization. To avoid this complication as much as possible, it is imperative that patients stop smoking for at least 1 month before and after the procedure. It is also important to avoid tension during closure, and to place the nymphoplasty scar as far forward as possible when the wedge technique is chosen, to avoid cutting the arterial branch vascularizing the central portion of the labia minora.
Hematomas may occur within the first 24 to 48 hours. They may be revealed by swelling or asymmetric pain.
Infection is uncommon, but can occur. It should be treated with appropriate antibiotic therapy.
Altered sensitivity is exceptional but can occur, and it is important to warn patients of this possibility. The same applies to hypersensitivity of the free edge in linear resections. To avoid this complication, it is useful to place the scar on the inner edge of the labia minora.
In rare cases, dyspareunia may occur, often linked to resections that are too large or exceed Hart’s line.
Bibliography
1. Hersant B, Jabbour S, Noel W, et al. Labia Majora Augmentation Combined With Minimal Labia Minora Resection: A Safe and Global Approach to the External Female Genitalia. Ann Plast Surg. 2018;80(4):323-327. doi:10.1097/SAP.0000000000001435
2. Goodman MP, Placik OJ, Benson RH, et al. A large multicenter outcome study of female genital plastic surgery. J Sex Med. 2010;7(4 Pt 1):1565-1577. doi:10.1111/j.1743-6109.2009.01573.x
3. Dubinskaya A, Dallas K, Eilber K, Scott V, Anger J. Female Genitalia in Pornography: The Source of Labiaplasty Trends? J Sex Med. 2022;19(4):S21-S22. doi:10.1016/j.jsxm.2022.01.051
4. Tepper OM, Wulkan M, Matarasso A. Labioplasty: anatomy, etiology, and a new surgical approach. Aesthet Surg J. 2011;31(5):511-518. doi:10.1177/1090820X11411578
5. Haylen BT, Vu D, Wong A. Surgical anatomy of the vaginal introitus. Neurourol Urodyn. Published online May 20, 2022. doi:10.1002/nau.24961
6. Botter C, Botter M, Pizza C, et al. The Suspensory Ligament of the Clitoris: A New Anatomical and Histological Description. J Sex Med. 2022;19(1):12-20. doi:10.1016/j.jsxm.2021.10.002
7. Furnas HJ, Canales FL, Pedreira RA, Comer C, Lin SJ, Banwell PE. The Safe Practice of Female Genital Plastic Surgery. Plast Reconstr Surg Glob Open. 2021;9(7):e3660. doi:10.1097/GOX.0000000000003660
8. Dayan E, Ramirez H, Theodorou S. Radiofrequency Treatment of Labia Minora and Majora: A Minimally Invasive Approach to Vulva Restoration. Plast Reconstr Surg Glob Open. 2020;8(4):e2418. doi:10.1097/GOX.0000000000002418
9. Alter GJ. Labia minora reconstruction using clitoral hood flaps, wedge excisions, and YV advancement flaps. Plast Reconstr Surg. 2011;127(6):2356-2363. doi:10.1097/PRS.0b013e318213a0fb
10. Jabbour S, Kechichian E, Hersant B, et al. Labia Majora Augmentation: A Systematic Review of the Literature. Aesthet Surg J. 2017;37(10):1157-1164. doi:10.1093/asj/sjx056
